天然木ローテーブル
(税込) 送料込み
商品の説明
5ほどで購入し5年間使用しました
大きな傷はありませんが表面に細かい傷はあります。
サイズは100*50*38cm タテ*ヨコ*タカサです。商品の情報
| カテゴリー | インテリア・住まい・小物 > 机/テーブル > センターテーブル |
|---|---|
| 商品の状態 | やや傷や汚れあり |

ローテーブル 幅100cm 木製 天然木 古材 正方形 ヴィンテージ調 ヘリンボーン テーブル ( 送料無料 センターテーブル リビングテーブル 机 パイン材 大型 カフェテーブル コーヒーテーブル オフィス 店舗 ディスプレイ おしゃれ ポイント消化 )

楽天市場】ウォールナット無垢材 天然木 センターテーブル 幅110cm

楽天市場】テーブル 無垢 座卓 150 テーブル 木製 ローテーブル 一枚板

天然木ローテーブル オープン×ストレージ(引出し1杯)タイプ|激安
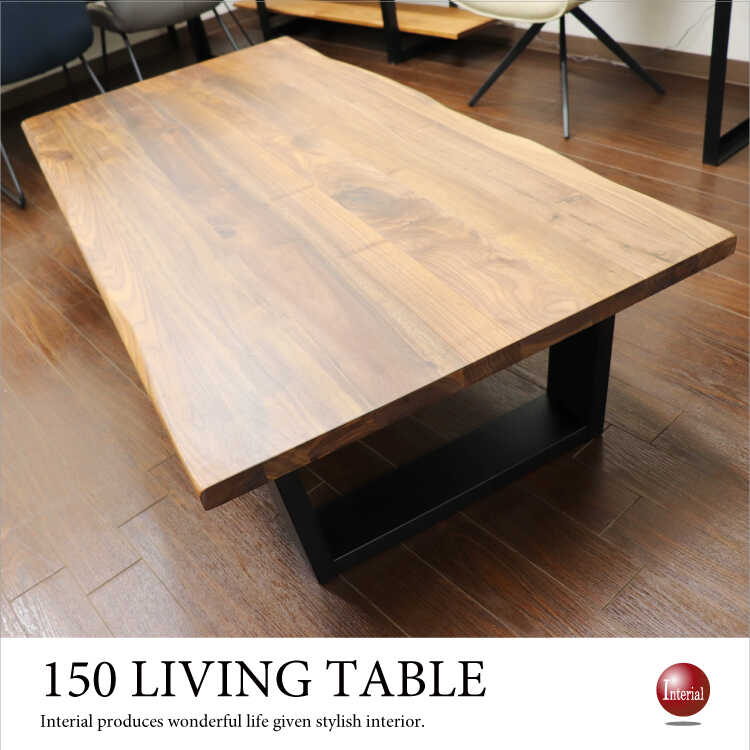
TA-2665 天然木ウォールナット無垢製ローテーブル|大きい150
テーブル おしゃれ 木製 古材 天然木 センターテーブル ローテーブル

リビングテーブル 木製 天然木 センターテーブル ローテーブル

楽天市場】センターテーブル 120 おしゃれ 座卓 高級感 無垢材 (流炎

楽天市場】リビングテーブル 引出し付きテーブル ローテーブル 北欧

ローテーブルケヤキ 天然木 無垢材 一枚板 | 木材・無垢材・一枚板

登場! 座卓 ローテーブル センターテーブル 柏木工 天然木 B061 飛騨の
テーブル 天然木 ローテーブル 円形 リビングテーブル 幅90 無垢 古材

第一ネット R337 天然木 センターテーブル、ローテーブル、幅110cm 手

高品質】 karimoku カリモク リビングテーブル シンプルモダン 高品質

おしゃれな木製テーブルが8000円以下から! | 【公式】LOWYA(ロウヤ

ローテーブル・リビングテーブル- 自然工房《国産・送料無料・開梱設置

センターテーブル 幅125cm 木製 天然木 古材 ヘリンボーン テーブル おしゃれ リビングテーブル ( 送料無料 ローテーブル 机 ソファテーブル 完成品 北欧 幅 125 カフェテーブル コーヒーテーブル リビング パイン材 ポイント消化 )

天然木 無垢材 センターテーブル リビングテーブル 丸机 円卓 オーク 新品登場

楽天市場】センターテーブル 120cm shape シェイプ ウォールナット

子供にやさしい北欧風ローテーブル 保育園にも納品実績あり。ひのき 天然木

注目の 天然木リビングテーブル センターテーブル - brightontwp.org

ローテーブル 丸 円形 座卓 1人暮らし ミニちゃぶ台 センター リビング ダイニング 食卓 国産ひのき 天然木 無垢材 おしゃれ 北欧 和風 子供部屋 ナチュラル シンプル | FLAILA interior(フライラインテリア) powered by BASE

角の丸みが優しい天然木テーブル 通販 - ディノス
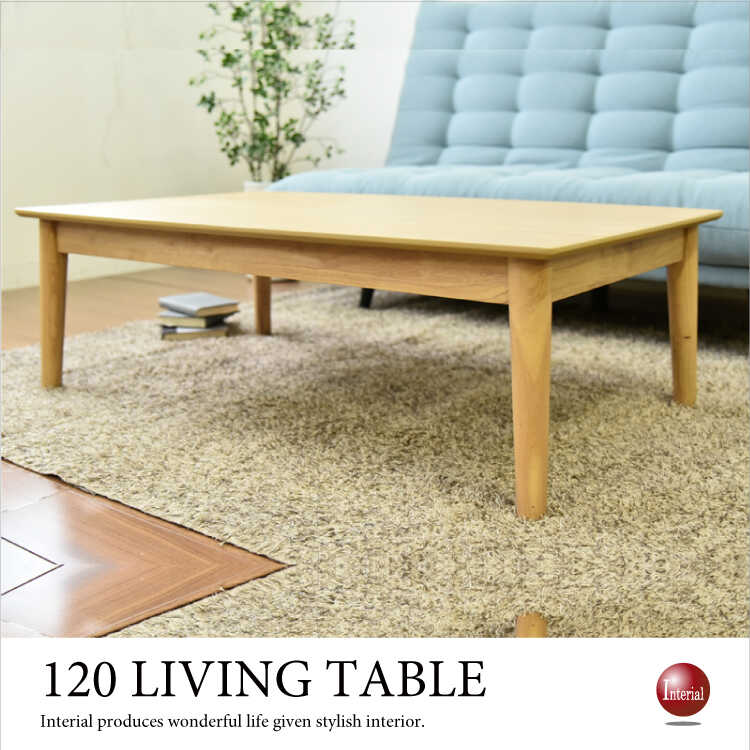
TA-2687 天然木オーク製ローテーブル|ナチュラル色・幅120cm
テーブル ローテーブル センターテーブル 105cm 木製 オーク 無垢

ローテーブル センターテーブル リビングテーブル 木製 収納付き
木脚を使ったそら豆のローテーブル【 Sサイズ】/ 天然木 テーブル

センターテーブル 天然木 テーブル ローテーブル リビングテーブル

無印良品 天然木 ローテーブル 廃盤商品 タモ材 MUJI ダイニング リビング 無印良品 新版

天然木センターテーブル LEANA(リーナ) 幅80cm | 【公式】 エア

ローテーブル リビングテーブル ひのき 天然木 MY 100 CT|家具の通販

【11月末で廃番】幅105cm 幅120cm タモ材 タモ無垢材 タモ天然木 木製ローテーブル ナチュラルテイスト シンプルモダン 収納棚付きセンターテーブル CURRENT - JOYSTYLE interior 本店

適当な価格 LOWYA ロウヤ テーブル ローテーブル 天然木 センター

天然木の折りたたみローテーブル / 90×45cm / ナチュラル / ウレタン

Amazon.co.jp: LOWYA ロウヤ センターテーブル テーブル ローテーブル

センターテーブル ローテーブル 木 長方形 ナチュラル 幅110×奥行50cm

アウトドアテーブル 天然木 折りたたみ ALT-01 キャンパーズ

ローテーブル 幅60cm 天然木 古材 センターテーブル リビングテーブル
![g78286]【幅100cm】 Giarmata センターテーブル 木製テーブル | 家具](https://d277jmppmje79i.cloudfront.net/uimg/g78286-l.jpg)
g78286]【幅100cm】 Giarmata センターテーブル 木製テーブル | 家具

送料込み】150×75オーク天然木 センターテーブル リビングテーブル 座卓-








商品の情報
メルカリ安心への取り組み
お金は事務局に支払われ、評価後に振り込まれます
出品者
スピード発送
この出品者は平均24時間以内に発送しています














